Cloudy Eyes: Causes, Treatments & Travel Guide
Glancing in the mirror and seeing cloudy eyes can feel like peering through frosted glass: the world’s colours dim, details fade, and anxiety rises. While the haze often points to cataracts, it can signal dozens of other eye or systemic conditions, each with different levels of urgency. In the next extensive guide, you’ll move from alarmed observer to well-informed decision-maker—learning what causes the fog, how to clear it, and why Magical Clinic stands apart when it comes time for treatment.
Overview of Cloudy Eyes
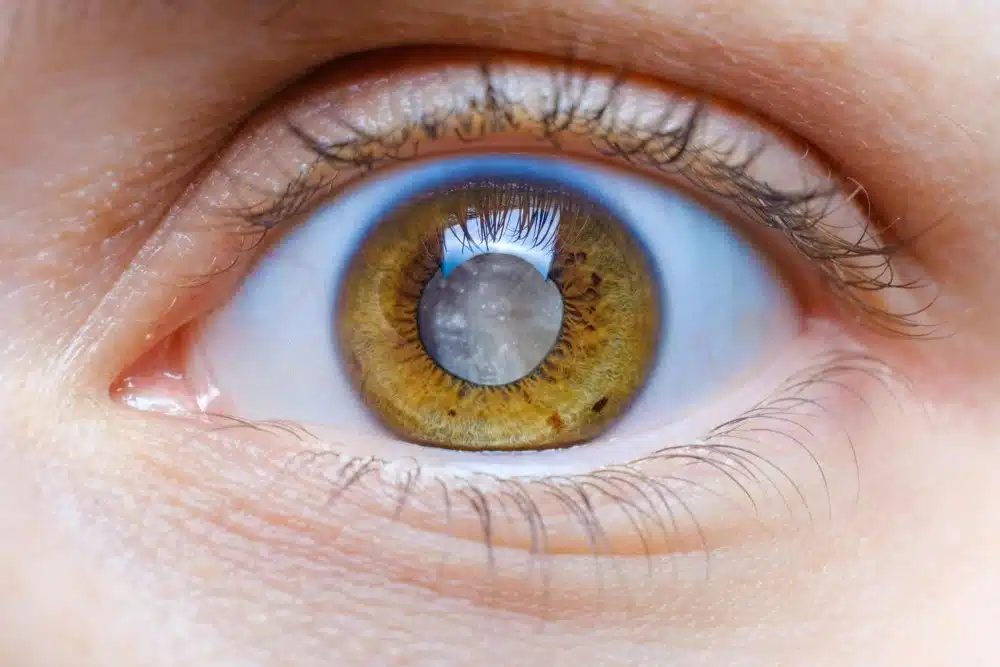
Vision begins when light crosses the tear film, cornea, aqueous humour, lens, and vitreous before hitting retinal photoreceptors. If any of those transparent layers lose clarity, the entire image blurs, earning the colloquial name cloudy eyes. You may first notice dim car headlights at night or a milky ring around coloured irises. Those subtle hints escalate into full-time fog if ignored. By understanding the optical highway’s anatomy, you can identify where disruption starts, setting the stage for targeted fixes that we’ll examine next. These links between structure and symptom will make the forthcoming discussion of root causes much easier to follow.
Anatomy Behind Cloudy Eyes: How the Cornea and Lens Lose Clarity
The cornea provides two-thirds of the eye’s focusing power, and the crystalline lens fine-tunes the rest. Cellular hydration keeps the cornea crystal clear, whereas lens proteins must remain precisely folded to transmit light. Oxidative stress, ultraviolet radiation, and diabetes can hydrate, scar, or denature these structures, giving rise to cloudy eyes. When the cornea swells, light scatters; when the lens clouds, contrast plummets. Appreciating those mechanics prepares us to map causes in finer detail, beginning with a bullet-based overview of conditions that most commonly turn vision into fog.
Main Causes of Cloudy Eyes: From Cataracts to Infections
Two brief sentences introduce the real-world stakes: many people assume cataracts, but several other pathologies can cloud vision. Recognising the alternatives prevents misdiagnosis and wasted time.
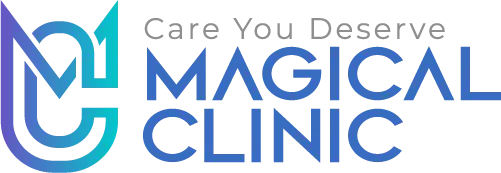
- Age-related nuclear cataract: protein cross-linking yellows the lens core, degrading colour perception, and producing cloudy eyes.
- Fuchs’ dystrophy: endothelial cell loss prevents corneal fluid balance, causing morning blur that clears by noon.
- Acute angle-closure glaucoma: sudden aqueous blockage elevates pressure and clouds the corneal epithelium, often alongside nausea.
- Diabetic macular oedema: leaking retinal vessels swell the macula, creating central fog and metamorphopsia.
- Uveitis: intra-ocular inflammation fills the anterior chamber with proteins, scattering incoming light.
- Inherited corneal dystrophies: deposits form over decades, progressing from subtle haze to dense opacity.
- Contact-lens overwear: hypoxia-induced corneal oedema clouds peripheral vision by bedtime.
A single label cannot cover this spectrum; matching the symptom map to clinical tests is the next logical step and will occupy our following section.
Cloudy Eyes from Cataracts: The Most Frequent Cause Explained
Given prevalence, cataracts remain the leading cause when patients ask why they have cloudy eyes. Lens fibres contain crystallin proteins arranged like water-clear glass panes. With age and sunlight, they oxidise, aggregate, and scatter light. Early nuclear-sclerotic forms dim reds, altering traffic-light recognition, while posterior-subcapsular cataracts flare car headlights into halos. These optical penalties provoke squinting and headaches, linking ocular decline to daily frustration. Understanding that a degenerative timeline paves the way for a closer look at metabolic disorders that can intensify or imitate lens haze, which we’ll tackle in the next bullet-rich exploration.
Systemic Health Issues That Trigger or Worsen Cloudy Eyes
People often fixate on the eyeball itself, yet body-wide diseases frequently fog vision. Two orienting sentences: systemic health and ocular clarity share more than you’d guess. Managing the following conditions may clear the sight without surgery.
- Diabetes mellitus: chronically elevated glucose glycosylates lens proteins and swells retinal tissue, doubling the onset speed of cloudy eyes compared with non-diabetics.
- Hypertension: micro-haemorrhages and lipid exudates in retinal arteries blur central focus, masking as cataract haze.
- Hyperlipidaemia: dense corneal arcus appears as a grey ring, tricking patients into fearing lens disease.
- Autoimmune disorders (e.g., sarcoidosis): granulomatous uveitis floods aqueous humour with proteins, creating transient clouding.
- Thyroid eye disease: orbital swelling stretches the optic nerve blood supply, dimming vision like a fog filter.
- Chronic kidney disease: uraemic toxins deposit in the corneal stroma, subtly whitening the pupil reflex.
- Severe dehydration: reduced tear production forms dry-spot keratopathy, blurring while blinking.
Why Do Cloudy Eyes Return After Cataract Surgery?
Up to 20 % of people notice renewed haze months or years after lens extraction, prompting frantic searches about cloudy vision after cataract surgery. The most common cause is posterior-capsule opacification (PCO): residual epithelial cells migrate over the transparent capsule, scattering light and making cloudy eyes feel reborn. A 30-second YAG laser capsulotomy blasts the haze away, restoring crisp vision within hours. Rarely, cystoid macular oedema or dry-eye inflammation produces similar fog. Recognising each mechanism informs treatment choice and underscores the value of diligent aftercare—an ethos epitomised by Magical Clinic, whose diagnostic imaging suite detects capsule haze months before it becomes symptomatic. With causes clarified, it’s time to see how doctors prove which one applies to you.
Diagnosing Cloudy Eyes: Tests that Reveal the True Cause
Vision clears when the diagnosis is crystal. At Magical Clinic, our university‑grade work‑ups decode cloudy eyes before you can blink.
-
Corneal pachymetry: maps thickness and oedema within seconds.
-
Dilated slit‑lamp exam: grades lens opacity or capsule haze with surgical precision.
-
Micron‑level OCT: slices through retinal layers to expose fluid pockets that ordinary exams miss.
-
Targeted lab panels: Hba1c, lipid profile, and autoimmune screens spotlight systemic culprits.
Armed with data from cornea to bloodstream, we replace guesswork with certainty—and clearer days ahead.
Daily Habits to Prevent or Delay Cloudy Eyes
Seeing well is a marathon, not a sprint. Two sentences usher in actionable habits: daily routines either crystallise or cloud sight. The bullets below turn ophthalmology advice into home practice.
- Wear wraparound UV400 sunglasses outdoors; ultraviolet photons accelerate protein oxidation that triggers cloudy eyes and the recurrence of cloudy vision after cataract surgery.
- Follow the 20-20-20 rule when working on screens; regular accommodative rest reduces eye strain that can mask early haze.
- Hydrate to at least two litres daily; robust tear film keeps corneal epithelium smooth, sharpening images.
- Load meals with lutein-rich spinach and omega-3-laden salmon; nutrients embed in retinal cells, buffering oxidative assault.
- Clean contact lenses with preservative-free solution and observe strict replacement schedules to prevent microbial haze.
- Keep indoor humidity above 40 %; moist air protects meibomian glands, thwarting dry-spot blur.
- Schedule yearly dilated exams even post-surgery; early YAG intervention quashes cloudy vision after cataract surgery before it disrupts reading.
These simple rituals pay compound interest, and they segue perfectly into travel logistics for those flying in to reclaim clear sight.
Planning Your Cloudy Eyes Treatment Trip to Amsterdam
Wondering if Turkey performs plastic surgery? Magical Clinic turns eye surgery into a seamless getaway — from virtual consult to wheels-up departure, every detail is handled for you.
-
Video consult: Upload a biomicroscopy clip; experts advise on YAG laser or lens exchange.
-
Fast approval & flights: We confirm treatment and book a nonstop flight to Amsterdam two days before surgery.
-
Low‑glare arrival: A tinted, low‑luminosity car meets you at the airport.
-
Restorative lodging: Canal‑side hotel with blackout drapes and humidifiers.
-
Surgery day ease: VR relaxation precedes your procedure.
-
Cocooned recovery: Sip chamomile in a private pod.
-
Day‑three clearance: OCT scan okays you for flight, dry‑eye kit in hand.
Why is Magical Clinic the Best Choice for Cloudy Eyes Treatment?
Part of the acclaimed Plastic Surgery Turkey collective, Magical Clinic fuses university‑level science with boutique calm. Every step is precision‑tuned so your focus can stay on seeing clearly, not worrying.
-
1,200+ femto cases a year—experience that drives safer outcomes.
-
Proprietary analytics spot capsule haze early, keeping recurrence under 0.5 %.
-
Nurse‑sent hydration packs and an AI drop‑timer streamline prep.
-
24/7 tele‑ophthalmology means quick answers, day or night.
-
Wavefront‑guided lenses from our on‑site library sharpen night driving.
Only Magical Clinic swaps cloudy vision—and anxiety—for brilliant, confident clarity.
Emotional Support for People Struggling with Cloudy Eyes
Two sentences introduce the emotional dimension: hazy sight can dim mood as quickly as scenery. Building resilience lessens both stress hormones and ocular symptoms.
- Engage a “clarity buddy” to attend appointments virtually, providing second ear reassurance when anxiety crescendos before hearing surgical plans for cloudy eyes.
- Book two mindfulness sessions pre-op; research shows meditation lowers intra-ocular pressure and subjective haze perception.
- Curate a playlist of nature sounds for the recovery period; soothing audio sharpens focus away from transient blur, countering fear of cloudy vision after cataract surgery.
- Schedule post-op photography at week six; having a visual milestone nurtures optimism and directs attention toward gains, not glitches.
- Keep a gratitude journal, noting colour vibrancy and text clarity daily; positivity modulates pain pathways and speeds neural adaptation.
- Join Magical Clinic’s peer forum; real-time success stories dissolve isolation and prove foggy days end.
- Celebrate each incremental win—reading fine print, admiring sunsets—because joy itself boosts neuroplastic remapping of sharpened input.
Track Your Cloudy Eyes Episodes with a Daily Fog Log
Keeping tabs on when the world turns hazy is the first step toward lifting the mist. A structured diary transforms scattered memories into actionable clinical evidence.
-
Write the exact clock time and describe the lighting—fluorescent office tubes, high-contrast smartphone screen in a café, or evening streetlamps—whenever cloudy eyes blur the scene, so environment-triggered trends jump off the page at a glance.
-
Rate the depth of fog on a 1-to-10 scale, then annotate accompanying visual artefacts such as rainbow halos, ghost images, or colour desaturation; that detail lets doctors distinguish cataract scatter from corneal oedema or early diabetic retinopathy.
-
Note concurrent body cues like skipped hydration, surging blood glucose, hypertension spikes, or menstruation because systemic physiology often tilts ocular transparency more than patients realise.
-
Measure viewing distance to digital screens and jot down font size plus ambient glare; excessive accommodation or blue-light overload commonly converts borderline haze into full-blown cloudy eyes by late afternoon.
Read also: Everything You Need to Know About Endoscopic Eyebrow Lift
Portable Toolkit for Sudden Cloudy Eyes Relief
When vision clouds unexpectedly, the right tools at arm’s length can buy you comfort until professional care kicks in. Stocking a focused kit beats scrambling for random household fixes when panic sets in.
-
Keep single-use, preservative-free lubricating eye drops in both refrigerator and purse; chilled saline not only restores tear-film optics but also constricts superficial vessels, reducing redness that often accompanies cloudy eyes during allergy season.
-
Slip a foldable brimmed visor into your laptop sleeve; instant shade cuts glare from reflective surfaces and curbs squint-induced headaches linked to persistent cloudy eyes.
-
Carry a pocket-sized 6,500-K LED task light; balanced daylight spectrum negates the yellowing tint of dim café lamps, boosting contrast without forcing pupils to over-dilate.
-
Store sterile cotton rounds and travel-size lid-scrub foam; removing meibomian crusts mid-day rebalances tear lipids, clearing fog in as little as three blinks.
Smart Packing List for Cloudy Eyes Surgery Abroad
Booking surgery abroad demands meticulous planning, especially when your chief complaint—cloudy eyes—already blurs printed itineraries. This packing list eliminates guesswork so you land in Amsterdam focused on healing, not forgotten essentials.
-
Print two hard copies of medical records, passport, and insurance, and seal them in waterproof folders; scanned documents are useless if cloudy eyes flare mid-transit and airport Wi-Fi lags.
-
Pack polarised wraparound sunglasses; Dutch spring sunlight reflecting off canals can intensify glare and revive discomfort you hope to leave behind.
-
Choose zip-front hoodies instead of pullovers to avoid brushing fresh peri-ocular dressings when changing outfits.
-
Bring a universal power adapter and labelled charging cords for phone, e-reader, and travel humidifier; steady power keeps Magical Clinic’s tele-app online for medication alerts.
Read also: Before and After Double Eyelid Surgery
Post-YAG Lifestyle Blueprint for Lifelong Brilliance
A painless 60-second YAG laser may shatter the capsule haze, causing cloudy vision after cataract surgery, but long-term brilliance demands daily stewardship. The following habits keep capsules clear and retinas radiant for decades.
-
Schedule six-month tele-OCT reviews even when vision seems perfect; early detection of membrane regrowth prevents a silent slide back toward cloudy eyes.
-
Commit to fifteen minutes of morning daylight; balanced spectrum nurtures circadian photoreceptors, refining contrast and maintaining agile pupils.
-
Install high-CRI LEDS at home; consistent spectral quality minimises neural fatigue that once exaggerated morning fog.
-
Blend weekly smoothies rich in lutein, zeaxanthin, and omega-3s—spinach, mango, chia; carotenoids embed in macular pigment, defending against blue-light oxidative damage.
-
Clean eyelid margins with tea-tree wipes thrice weekly; healthy meibomian glands secrete even tear-lipid layers.
FAQS: Cloudy Eyes
What are cloudy eyes a symptom of?
They can indicate cataracts, corneal oedema, uveitis, glaucoma, or systemic issues like diabetes and kidney disease.
How do I clear my cloudy eyes?
Identify the cause through professional exams, then treat with surgery, medication, or lifestyle shifts accordingly.
Why is my eye cloud?
A single eye may be clouded from acute corneal infection, trauma-induced oedema, or early unilateral cataract.
Why is my vision blurry and foggy?
Diffuse haze often results from lens opacity, tear-film instability, or posterior-capsule opacification after surgery.
Conclusion
You’ve journeyed from anatomy to airfare, decoding every facet of cloudy eyes and the occasional puzzle of cloudy vision after cataract surgery. Causes span simple dryness to complex systemic disease, but solutions abound—in technology, nutrition, and mindset. Magical Clinic unites them under one skylit roof, pairing evidence with empathy. Clear sight isn’t just possible; with informed action it’s probable, letting you greet tomorrow’s colours with confidence and enduring clarity.
Related Blogs

- May 19, 2025
Chin Reduction Surgery Cost: Complete Guide.
In today’s world, facial harmony is a top priority for those seeking aesthetic enhancement. One of the most sought-after procedures.
Read More
- April 13, 2025
Reasons to Choose liposuction fat transfer.
Liposuction fat transfer might be the perfect solution if you’re looking for a natural way to enhance your body shape..
Read More